Glaucoma Cases
A True Story 1:
* Patient has kindly given consent to this articleMadam S was diagnosed as Primary Open Angle Glaucoma at the age of 38 year-old.
She was referred to me in year 2013 (Age 42) for uncontrolled IOP of her left eye with maximum topical & systemic eye pressure lowering medicines. She also had a failed Trabeculectomy in her right eye in year 2008 done by a local private general ophthalmologist.
At presentation; her eye pressure was 20mmHg for her right eye; Left eye was 40mmHg with 4 glaucoma eyedrops in addtion to maximun dose of Tab Diamox & IV Mannitol. However, her visual acuity was still good 6/6 Snellen both eyes.
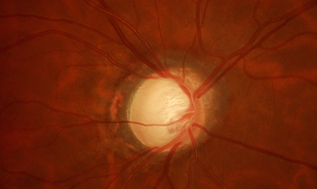
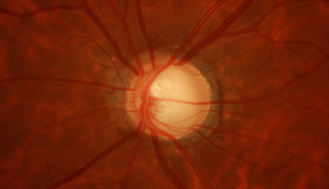
* Picture taken on Dr Lee's patient with consent
Fundus Photograph:
Humprey Visual Field Test (year 2013)
> both eyes constricted visual field - patient had tunnel-vision
She underwent Trabeculectomy for her left eye in April 2013
Post-operatively her left eye’s pressure was stable around 14-18 mmHg with no eyedrops.
Left Eye - Post Trabeculectomy
During her regular followup subsequently, she was adviced for Glaucoma Tube-Shunt Surgery for her right eye (with a failed trabeculectomy) as her IOP was not well controlled. It fluctuated between 23 to 27 mmHg with 4 glaucoma eyedrops. However, the patient was not keen as she could not find suitable times for surgery.
In Dec 2014, she came back to me with right eye’s IOP of 38mmHg. Her visual field had deteriorated significantly at that time.
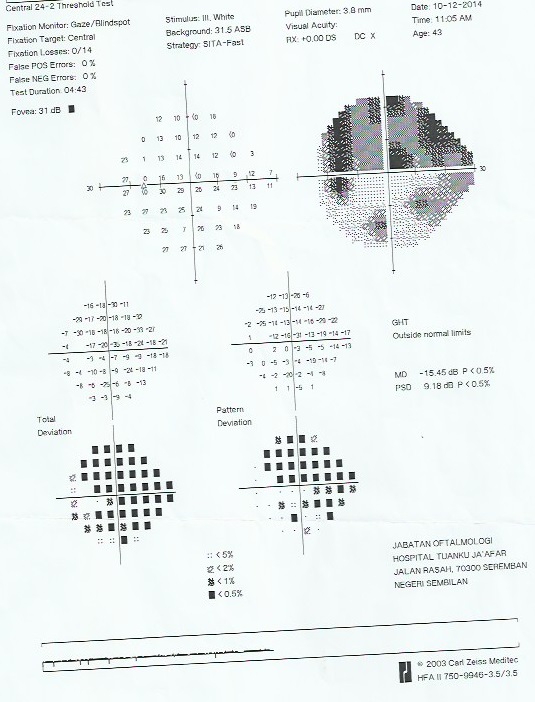
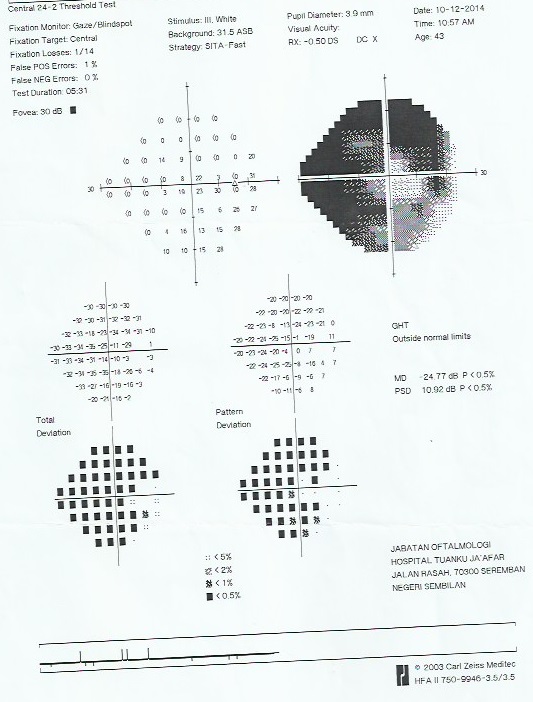
Humphrey Visual Field Test (Year 2014):
> Her right eye’s visual field had constricted further. Her left eye’s visual field was stable although her vision had dropped to 6/12 because of the emergence of cataract.She was scheduled for Glaucoma Tube Shunt Surgery with Baerveldt Glaucoma Drainage Device for her right eye in Dec 2014.
Phacoemulsification cataract surgery with implantation of artificial intra-ocular lens (monofocal) for her left eye in March 2015. During her cataract surgery, she was given subconjuntiva 5FU to prevent scarring of her trabeculectomy site.
In July 2015, her right eye’s IOP was 17mmHg and Left eye was 15 mmHg with no glaucoma eyedrops. Her visual acuity was good; both eyes read 6/6 Snellen.
However, her right eye’s IOP was rising with time and she had to put back on one glaucoma eyedrops later. At her last review in August 2017, her right eye’s IOP was recorded at 18 mmHg while her left eye remained good at 12 mmHg with no glaucoma eyedrops. Visual acuity was still good for both eyes; she read 6/6 Snellen unaided.
Glaucoma causes irreversible loss of the optic nerve. Although we can’t bring back the dead nerve fibres, we could prevent further loss with IOP lowering medications and glaucoma surgeries. This unfortunate lady had obviously benefitted from early treatment. Without the early interventions with Glaucoma Surgeries, she would have gone blind at the age of 42.
Humphrey Visual Field Test (Year 2017):
> Both eyes’ visual field showed no further progression
Left Eye 24-degree view |
Right eye 10-degree view |
Patient continued her regular clinic visits in a government hospital. She would come to see me when her IOP was not well controlled. According to her, her right eye’s treatment had been increased to 4 anti-glaucoma (maximum) eyedrops since Jan year 2020 and her IOP was still not good. It measured above 20 mmHg. Visual Field test showed worsening of visual filed in both eyes. However, her left eye’s IOP remained good with no medications needed.
Humphrey Visual Field Test (Year 2020):
Left Eye 24-degree view |
Right eye 10-degree view |
Fig: Right Eye
|
Fig: Left Eye with a good Bleb on top covered by upper eyelid |
|
|
Her IOP: Right Eye 20 mmHg , Left Eye 12 mmHg when she revisited my clinic in Feb 2020. Her visual acuity was RE 6/9; LE 6/6. Left eye was medication-free. IOP of 20 mmHg was a bit too high for her right eye in the presence of advanced optic nerve damage. I had thus advised her for Cyclophotocoagulation laser treatment on her right eye to reduce IOP. I had also warned her that we may need a second Glaucoma Tube Shunt surgery if the IOP rise again.
Madam S continued her follow-up with me and also in general hospital near her home. Her right eye’s pressure was on the rise again despite on maximum topical eyedrops. She came to me again in Nov 2020 with her right eye’s IOP 23mmHg. Her left eye which had trabeculectomy in 2013 remained good with IOP 11 mmHg. She was advised for micropulse transscleral cyclophotocoagulation which is a form of minimally invasive glaucoma surgery(MIGS) and it was done immediately. He right eye’s IOP was eventually stabilized around 16 mmHg with Ganfort nocte, Alphagan tds and azopt tds. Visual acuity was RE 6/15, pH 6/12 and LE 6/6. However this only worked for about 9 months and her RE’s IOP started to creep up again to 22mmHg on her clinic visit in Aug 2021.
After long discussion and informed consent about risk of surgical complications like hypotony, choroidal detachment and blindness, Madam S agreed for a repeat Trabeculectomy on 10th Sept 2021. We knew we were working against the odds to save her vision. The surgery was difficult in the presence of extensive conjunctiva fibrosis with old failed trabeculectomy and tube. I was relieved that the surgery went well and all her glaucoma eyedrops was stopped immediately postoperative. She recovered well and the shunt was working well. Her RE’s IOP was lowered and recorded at 8 to 10 mmHg during her post- operative follow up and her RE’s visual acuity improves to 6/9. It is encouraging to see this very good surgical outcome despite her very advanced disease. It is a known fact that the risk of vision ‘wipe-out’ is very high for advanced glaucoma during and immediate after glaucoma surgeries. Decision on surgical intervention at this stage could be a dilemma and thus a high risk informed consent from patients is usually required.
I last saw her on 7th Feb 2023, Her visual acuity was RE 6/9, LE 6/6. IOP RE 10mmHg and LE 12 mmHg with no glaucoma eyedrops needed in both eyes.
Shunts/Tubes implanted during Glaucoma Surgeries may become obstructed with times due to tissue fibrosis/scarring. The younger the patient is, the stronger the scarring response. Other factors like lids or conjunctiva infections or inflammation would accelerate scar formation. Thus lids hygience and regular follow up is essential to ensure the shunt/tube working well. Sometimes, needling of bleb/tube could help to resuscitate a failing bleb/tube.
Madam S is 51 year-old at this point of time. She will have another 30-40 years to go (according to normal life expectancy). We should continue to take care of her eyes; to keep her remaining optic nerve healthy and thus to prevent blindness. It’s a known fact that Glaucoma is a progressive neuro-degenerative disease. Prevention of blindness at this advanced stage particularly is an uphill task.
Although It had been a tedious work fighting against visual loss for this patient; it is definitely worthwhile as we could preserve her vision.
Humprey Visual Field Test (year 2022)
This visual field test analysed the central 10-degree of her vision. Both eyes visual field are constricted. Although she still read 6/6 (Snellen Visual Acuity Chart) for right and left eye; the quality of vision in her left eye is better.
Left Eye 10-degree view |
Right eye 10-degree view |
A True Story 2:
* Patient has kindly given consent to this article
Mr X was a 62 year-old retired Bank Manager, a known case of Primary Open Angle Glaucoma since year 2008 when he first presented to me in year 2012 in Hospital Kuala Lumpur. He had undergone Glaucoma Surgery / Trabeculectomy in both eyes consecutively in year 2010 by a private general ophthalmologist but unfortunately both of the surgery had failed. He was restarted on glaucoma eyedrops in the same year.
At presentation, his Right eye’s IOP was 18 mmHg and Left eye was 28 mmHg. Both eyes had good visual acuity of 6/9. At that time, he was treated with Xalatan and Timolol eye drops.
Humphrey Visual Field Test (Year 2012):
Left Eye 24-degree view |
Right eye 24-degree view |
He was advised for Glaucoma Filtering Surgery/Trabeculectomy augmented with Mitomycin-C on his more severe left eye in December 2012.
Fig: Bleb appearance on Week-1 post-surgery; IOP 15 mmHg |
Fig: Nice Bleb on Month-3 post-surgery; IOP 9 mmHg |
His left eye’s IOP was reduced to 10-12 mmHg after surgery with no glaucoma eyedrops needed. He was then advised for Glaucoma Filtering Surgery/Trabeculectomy on his right eye. However he had chosen to delay surgery at that point of time.
In year 2015, he came to see me in ParkCity Medical Centre with Right eye uncontrolled IOP. His visual field had shown progression/worsen over times and he was put on maximum (4) topical eyedrops.
Humphrey Visual Field Test (Year 2015):
Left Eye 24-degree view |
Right eye 24-degree view |
He soon underwent Glaucoma Filtering Surgery/Trabeculectomy augmented with Mitomycin-C on his right eye on the same year (2015).
Fig: Right eye; Nice Bleb 2 year post-surgery; IOP 10 mmHg |
Fig: Left eye; Nice Bleb 5 year post-surgery; IOP 10 mmHg |
Thereafter, his IOP had been good and he did not need glaucoma eyedrops anymore (left eye since year 2012 and right eye since year 2015). His IOP readings were around 10-12 mmHg during his many clinic visits with me till today.
The latest visual field test was done in Feb 2020; it showed improvement of visual function. His visual acuity was good, Right Eye 6/6 Left Eye 6/9 and IOP was 10 mmHg in both eyes on his last clinic visit in Feb 2020.
Humphrey Visual Field Test (Year 2020):
Left Eye 24-degree view |
Right eye 24-degree view |